Treatment and Management of Parkinson’s Disease
This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
What is the main treatment for Parkinson's disease?
Medication is the main treatment for Parkinson’s disease. Medications your doctor prescribes will likely help your Parkinson’s symptoms, but they also can cause side effects, and some medications become less effective over time.
Parkinson’s treatment has two goals: The first is to manage your symptoms as well as possible. The second is to minimize side effects of treatment.
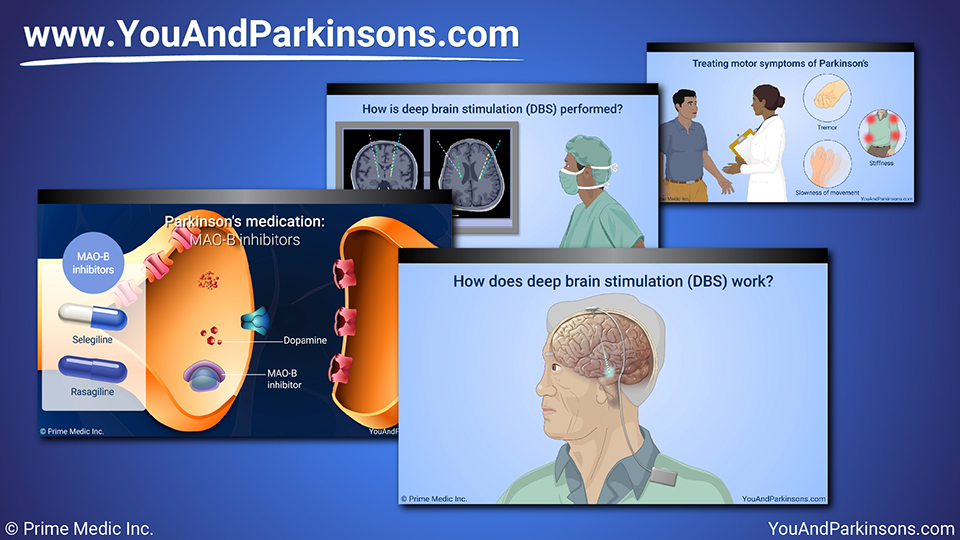
Treating motor symptoms of Parkinson’s
Parkinson’s causes movement – or motor – symptoms, and non-motor symptoms.
Medication can often control motor symptoms for many years. These symptoms include tremor, stiffness, and slowness of movement.
Your doctor will probably need to adjust your medications over time. It’s important to tell your doctor about all your symptoms and even keep a daily record, or diary, of how you feel. This will enable more effective medication adjustments.
Parkinson's medications
The medications you take for early Parkinson’s may be different from those you take later. There are three main medication classes for Parkinson’s:
- Dopamine agonists;
- MAO-B inhibitors; and
- Levodopa.
The decision as to which class to begin treatment with will depend on your age, symptom severity, and the potential side effects of each medication.
These medications help simulate, extend, or replace, respectively, the brain chemical, dopamine, which is reduced in Parkinson’s disease.
Parkinson's medication: Dopamine agonists
Dopamine agonists cause dopamine-like effects in the brain. These include pramipexole, ropinirole, and rotigotine transdermal patch.
Parkinson's medication: MAO-B inhibitors
MAO-B inhibitors keep the brain from breaking down its natural dopamine quickly. They include selegiline and rasagiline. They can be effective for early, mild symptoms.
Parkinson's medication: Levodopa
Levodopa helps replace dopamine in the brain.
All Parkinson's disease patients eventually take carbidopa-levodopa – or levodopa for short – which is the gold standard treatment.
Parkinson's medication: Levodopa
Several forms of levodopa are available. You can take:
- An immediate release tablet that gives all the medicine at once;
- A tablet that releases medicine over a longer time; or
- A dissolvable tablet you can hold on your tongue, to take without water.
Motor complications of Parkinson’s: Levodopa wearing off episodes
Over time, with disease progression, Levodopa’s effects can wear off faster. During these periods, patients may feel their motor symptoms return prior to their next dose.
Therapeutic options your doctor may consider include changing the frequency of your levodopa dose or adding levodopa-extending drugs such as entacapone or a MAO-B inhibitor (such as rasagiline or selegiline).
Motor complications of Parkinson’s disease: Levodopa-induced dyskinesia may develop with long-term use of levodopa
Too much levodopa tends to produce abnormal involuntary movements called “dyskinesias”. Your doctor will try to help you balance “on” times, when you have well-controlled symptoms and little non-bothersome dyskinesias, with “off times” when your medication levels are low and Parkinson’s symptoms bother you.
Therapeutic options your doctor may consider include: reducing your levodopa dose or frequency, or adding amantadine.
Treating non-motor symptoms of Parkinson’s
Many non-motor symptoms can be treated individually. For example, your doctor can recommend other medications for constipation, sleep issues, or depression. Again, writing down your symptoms can help you get the necessary treatment.
Failure to treat these symptoms can worsen the motor symptoms of Parkinson’s disease.
Parkinson's surgery: Deep brain stimulation (DBS)
A surgical treatment called deep brain stimulation (or DBS) should be considered for motor complications that are not improving significantly with medication adjustments. DBS treats problems such as tremor, stiffness, and slowness of movement.
How does deep brain stimulation (DBS) work?
DBS involves placing tiny electrodes into specific areas of the brain. They are attached to a battery-powered stimulator under your collarbone.
Your doctor can adjust the stimulator to deliver electrical signals that will help alleviate the movement problems.
How is deep brain stimulation (DBS) performed?
DBS is done in a hospital, after careful evaluation by a neurosurgeon. In the past, patients had to be awake for the procedure. Now, experts can do “asleep DBS,” using advanced imaging to identify where the electrodes should go.
Will deep brain stimulation (DBS) work right away?
Your DBS will probably not give perfect relief right away. Your medical team will adjust it over a period of months for the most benefit.
New treatments for Parkinson's
One new medication is a gel form of levodopa that goes directly into the body through a small pump. Research shows it can give more “on” time with fewer abnormal movements than immediate release levodopa tablets. Ask your doctor about other new treatments.
Complementary and supportive therapies for Parkinson's
Beyond surgery and medication, it is vital to
engage in:
- Regular exercise;
- Physical therapy for movement problems;
- Speech therapy for voice and swallowing problems; and
- Counseling and medication for depression.
Complementary and supportive therapies for Parkinson's
Massage, acupuncture, yoga, and other body care practices may also help.
A diet consisting of plenty of fruits, vegetables, and water can help with Parkinson’s-related constipation. Protein may be a concern in your diet at different stages of Parkinson’s, because with some people it can interfere with how your medication is absorbed. A nutritionist can help you find the right balance.
What other treatment options are available for Parkinson’s?
Researchers are working to find new Parkinson’s treatments. Clinical trials – which are research studies done with volunteers – are underway for gene therapy and medications to slow the loss of dopamine-producing nerve cells, as well as other Parkinson’s treatments.
Managing Parkinson's medications
Ask your doctor about clinical trials. You may help your own disease, and you will give doctors valuable information on future treatments.
Taking your medications as directed, telling your doctor about symptoms and possible side effects, and asking questions can make your treatment more effective. If one Parkinson’s medication does not help, you still have other options.
Managing Parkinson's medications
Seeing your doctor every 3 to 6 months, having your medications adjusted regularly, and telling your doctor about changes and side effects are important in Parkinson’s disease.
What can I do to best manage my Parkinson's disease?
You can do a lot to manage this lifelong disease and have a good quality of life.
Finding the right doctor and working with them to take the best care of yourself can give hope and help you live well with Parkinson’s.